After such an atypical year, writing a typical year-end review feels strange. Some of us now reflect on 2020, while others seek to blot it from their memories. We feel both excited and relieved to flip the calendar to 2021 after the unthinkable, COVID-19-ridden year we endured. The pandemic spanned the globe and, in the process, infiltrated nearly every aspect of life.
Last year at this time, we wrote about regulatory shifts, elections, and disruptive and innovative momentum that was sure to impact our daily lives through the healthcare industry. While these largely came to fruition, the pandemic altered the trajectory and became an unexpected catalyst. Looking ahead to 2021, we anticipate several key themes and trends continuing to grow at break-neck speeds. COVID-19 acted like an earthquake on the industry, causing a few tsunami-like waves that disrupted the typical pace of innovation. Topics typically confined to scientific journals and hospital hallways became commonplace on nightly news and at family dinners.
As we enter 2021, we contemplate a world in which no facet of the previous healthcare structure is deemed unchangeable. 2020’s undeniable impact will continue into the new year as the wave of change, innovation and adaptability washes over the industry:
 Unprecendented Growth Accelerates Innovation
Unprecendented Growth Accelerates Innovation
COVID-19 ignited a massive increase in demand for telehealth services, which peaked during widespread shutdowns in April, but today remains well above pre-pandemic levels. As a percentage of office visits, telehealth visits attributed for less than 1% of visits pre-pandemic;
this peaked to almost 50% during April and now sits around 11% of total visits. Previously impeded by an unfriendly regulatory environment and consumer doubt, telehealth had grown steadily, but slowly. CMS’s most recent fee schedule made the temporary reimbursement changes permanent, solving a key problem previously prohibiting broader adoption (after all, providers have P&Ls too). Telehealth offers better population health outcomes via increased access and reduced variability of care, which has widespread buy-in from both consumers and providers. The question is no longer whether telemedicine is “real” healthcare, but rather, what is the optimal mix of in-person versus remote services that achieves the triple aim.
Telehealth’s buy-in from both providers and patients increased substantially, even before the new reimbursement structure became finalized; a recent study of U.S. consumers suggests that approximately
80% of patients who tried telehealth during the pandemic plan to utilize it post-pandemic. Routine primary care is clearly well-positioned to be a long-term and high-volume user of telehealth, but other modalities are increasing their use as well. Mental and behavioral health services are increasing access to care for the ongoing mental health crisis in America (discussed below). Additionally, telepsychiatric services for more severe mental health episodes are seeing increasing telehealth use at hospitals and health centers without in-person psychiatric staff.
.png)
Healthcare delivery can and will travel with us, in our pockets, wherever we go. Although higher acuity services still cannot be provided remotely, a greater understanding of which parts of the care process can be managed remotely is changing rapidly.
Technology will Continue to Drive Healthcare to the Home
As discussed in our healthcare at home blog post, the home is an incredibly valuable clinical setting for patients, who prefer to receive care in their own homes, as well as payers, that benefit from a lower total cost of care than in traditional settings. As a result, providers have a growing interest in pursuing an in-home care ecosystem approach that allows a more holistic set of care solutions including: preventative measures (remote patient monitoring), ancillary care delivery in an in-home setting (skilled and non-skilled home health, hospital-at-home models, and behavioral health), and supportive solutions (nutrition assistance, medication delivery / reconciliation, and durable medical equipment). The global pandemic likely shifted the paradigm of primary care permanently by accelerating the adoption and innovation of both telehealth and telemedicine. Given the existing tailwinds for this market coupled with a global drift towards digitization, we expect the following virtual care trends to continue in 2021:
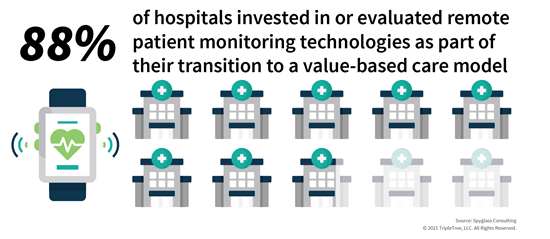
- Increasing Reliance on Remote Patient Monitoring. As of late 2019, approximately 88% of hospitals invested in or evaluated remote patient monitoring technologies as part of their transition to a value-based care model. With tools like the Apple Watch and Fitbit becoming more ubiquitous, remote patient monitoring will continue to play an important role to help monitor and treat the increasing population of patients suffering from chronic conditions, including cardiovascular disease and diabetes.
- Continued Utilization of Telehealth. As mentioned above, COVID-19 provided a much-needed catalyst for the widespread utilization of telehealth services. On March 17, CMS released a waiver allowing expanded telehealth services under Medicare. Following this waiver, we observed large insurers such as Blue Cross Blue Shield, Humana and UnitedHealthcare expand coverage. To end the year, CMS finalized permanent expansion of telehealth under Medicare, adding 144 different services. COVID-19 quickly proved that telehealth is a viable care delivery platform, and one that is more time-efficient for providers and more cost-efficient for payers. As we enter 2021, we expect to see utilization of telehealth continue both during and after the current pandemic.
- Telemedicine is Here to Stay. A study of ~16mm Americans found that their use of telemedicine increased ~20x between January and June of 2020. As care delivery continues to shift to the home, providers will continue to prescribe medicine virtually, relying on remote patient monitoring and other provider technology to make more educated care delivery decisions.
Government Populations Continue to Rise
Last year, we wrote about the explosive growth in Medicare Advantage (MA) plans. This growth is expected to continue, as an aging boomer population, combined with increasing popularity of managed care and value-based contracting, encourages MA enrollment. Total enrollment is nearing 25 million, which equates to 40%+ of Medicare
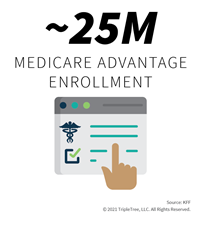
beneficiaries, up from 34% in 2019. If the COVID-19 pandemic was not enough, 2020 also witnessed an election that will bring a new administration to the White House and new priorities to government-sponsored healthcare programs.
Perhaps the largest shift in momentum within government programs is Medicaid,
a topic we wrote about in 2020. After three consecutive years of declining Medicaid enrollment, from 2017 through 2019, COVID-19’s impact on the economy and consequently, the Medicaid-eligible population, has been substantial, with at least five million Americans added to Medicaid rolls this year. The need for change in managing and paying for the Medicaid population is clear. Given low reimbursement rates, providers are often hesitant to treat Medicaid patients, resulting in significant wait times (sometimes weeks) for patients seeking care. Historically, Medicaid populations have struggled to achieve comparable health outcomes to commercial, Medicare, and sometimes even uninsured populations.
Managed Medicaid covers north of 60 million Americans today, equating to ~2/3 of total Medicaid enrollees. Total Medicaid enrollees are up from ~75 million pre-COVID-19 to 90 million currently. Tightening state budgets, greatly exacerbated by the pandemic, have driven states to seek risk-based contracting arrangements. This approach adds greater predictability to budgets and shifts financial risk to the Medicaid MCOs ultimately managing the population. Risk-bearing financial arrangements carry huge advantages in their ability to save money given both the impact of co-morbidities and the likelihood that Medicaid enrollees suffer from multiple conditions. More proactive management of high-cost Medicaid patients can potentially remove enormous costs from the system, not to mention the increased productivity possible for working-age populations that spend less time needing medical care.
Self-Funded Employers Will Continue to Drive Innovation
As we observe healthcare trends at the beginning of the year, one fact remains constant: the method in which healthcare is priced and paid for in the U.S. is not sustainable. Many attempts to curb healthcare costs have been taken by providers, employers, and insurers, but healthcare costs continue to increase at higher rates than inflation and wage increases across the country. For example,
the average single and family premiums increased 4.0% over the past year, compared to increases in workers’ wages and inflation of 3.4% and 2.1%, respectively.
Self-funded employers have the power to make healthcare more affordable for both employees and the c
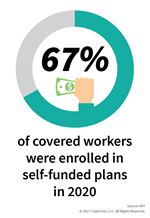
ompany. During 2020,
67% of covered workers, including 23% of covered workers in small firms and 84% in large firms, were enrolled in self-funded plans, which represents an increase of 6% from 2019. Moreover, in 2020 we tracked ~25 employer-based M&A transactions, which represents a 92% increase from the prior year. These acquisitions included companies specializing in reference-based pricing (RBP), population health applications, care navigation, pharmacy benefit management, and other health plan administration services. Given the increasing importance of self-funded employers to healthcare and the overall economy, we expect to see the following trends continue to evolve during 2021:
- Emphasis on physician quality. Health plans are limited in their ability to steer individuals to the highest quality providers for fear of network friction. Frustrated with this lack of quality and cost management, employers are seeking independent vendors that can integrate for member navigation. We expect vendors across the cost containment spectrum to continue incorporating quality metrics into their solutions, including second opinion solutions, physician quality scoring, and centers of excellence.
- Improved pharmacy cost containment. Pharmacy costs continue to be a rapidly growing component of medical spend, especially for employer-sponsored health plans. Additionally, large pharmacy benefit managers (PBM) provide poor member and utilization management services and do not focus efforts on mid-size and smaller employer groups. To combat this, employers are more actively carving out the pharmacy benefit to participate in aggregation models to bring both purchasing power and more focused clinical services.
- Advanced specialty condition management. We have observed a growing popularity for niche solutions that focus on small, but very high-cost employee populations that drive a meaningful portion of overall healthcare spend. With strong technology foundations and advanced data analytics capabilities, specialty condition management platforms can create very individualized experiences for employees while equipping employers with quantifiable ROI tracking to offer differentiation from traditional wellness solutions.
- Modern tools enabling employees to better utilize and navigate their benefits. Beyond providing a better healthcare benefit, we have seen significant demand for capabilities that can enable better access, knowledge, and understanding of the resources employees have at their disposal. From physician quality navigation, to second opinions and clinical guidance, to an e-commerce shopping experience for products and services eligible under the healthcare benefit, employers are seeking ways to drive engagement and utilization of the benefits while effectively managing costs.
Behavioral Healthcare Will Remain Attractive
The behavioral healthcare market entered 2020 with significant momentum as sweeping de-stigmatization of mental health continued. Existing demand for behavioral healthcare services skyrocketed during the pandemic as substance abuse, alcoholism, and suicide rates all increased. Given most Americans have behavioral health coverage from mental health parity and the Affordable Care Act, the demand for these services will continue to be strong in 2021.
According to a
2019 market study, the annual behavioral health market is projected to reach $240B+ by 2026.
.png?width=275&height=218) With nearly 80% of adults in America reporting significant stress related to COVID-19
With nearly 80% of adults in America reporting significant stress related to COVID-19, existing behavioral health patients and a rising tide of new “entrants” across the severity spectrum will continue to seek behavioral care. Additionally,
there are ~6,000 too few behavioral health providers in the U.S.; the shortage is expected to grow to 250,000 by 2030. Given these market statistics, we expect to see the following trends continue to take place during 2021:
- Increased access to care. As the stigma around behavioral health conditions continues to fade and the broader healthcare industry’s focus on behavioral health intensifies, we expect to see sustained efforts from the government and the private sector to drive increased awareness and further expand access to care. Increased adoption and utilization of telehealth and telemedicine services lowers the barrier to seeking care for behavioral health services, as the country navigates the pandemic and mental health crisis.
- Growing demand for new solutions. Significant capital has been invested into digital health platforms, spanning providers, employers, payers, and direct-to-consumer. The rapid growth of segment-specific behavioral health services is driving demand for new provider IT solutions / platforms with behavioral health technologies spanning core EHR/PM infrastructure, to telehealth platforms, to consumer applications for self-help. Over the past 3 years, we observed 25+ behavioral health technology M&A transactions. We expect to see continued interest from both strategic and financial buyers in this space.
- Steady investment from private equity. Over the past two years, we observed the formation of ~60 new behavioral health private equity platforms. Given the significant tailwinds heading into 2021, we expect private equity investors to continue playing a large role in the behavioral healthcare market.
We are excited to observe the rising wave of change, innovation and adaptability progress throughout the year and look forward to (re)connecting with many of you as travel allows. In the meantime, let us know what you think. Wishing you a happy, healthy, and successful 2021!