(Our post last week on Duals created some great dialogue. Since its publication, we have been in strategic road mapping sessions with both a large commercial payer, and a major healthcare delivery system — the dual eligible opportunity constituted a large part of these discussions. It is quite clear that while CMS is working to get its dual demonstration projects mapped out and launched, there is a tremendous need in the market place to more effectively (both in terms of quality and cost) manage care in the Medicare and Medicaid programs. This is especially true for the Dual Eligible populations. Given the pace of our conversation around dual eligibles, we’re expecting a continued focus on this area in the near term and wanted to offer some additional insights below.)
Dual eligible individuals qualify for both Medicare, a federal health benefit program primarily for those who are disabled or over 65, and Medicaid, a state health benefit program for those who fall under a given state’s poverty level designation. Almost all dual eligible individuals have low or no incomes, with nearly 90% being far below the federal poverty level. Besides being poor, the dual eligible population has other unique socio-demographic characteristics. Compared to the Medicare population, they are disproportionately female and in minority groups, with many being African American or Hispanic. More than half are not high school educated, have limited English language skills, and live alone.
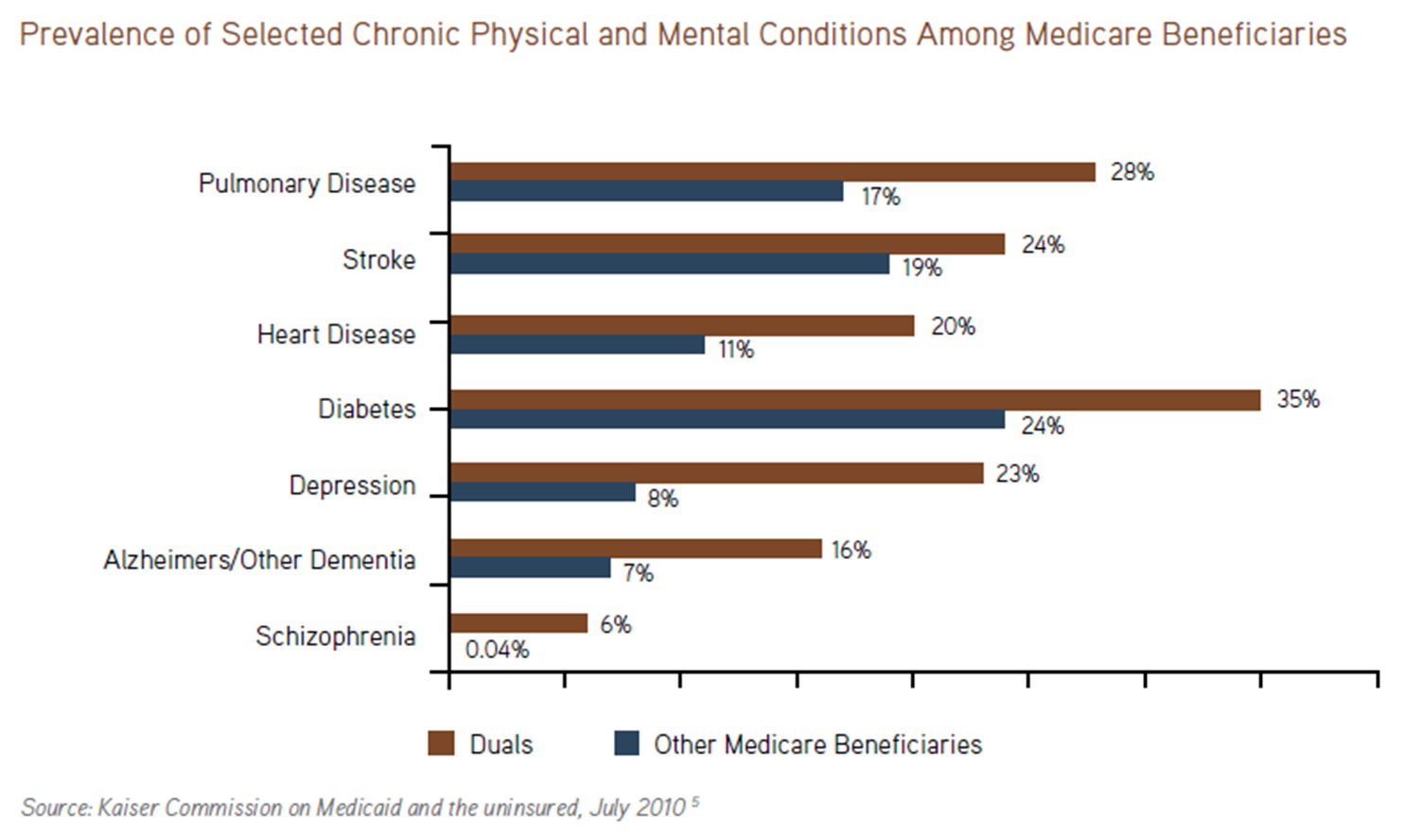
In addition, many are disabled (physical or mental) with complicated health conditions. Kaiser Family Foundation reports that nearly 40% of duals suffer from both physical and mental diseases, and these co-morbid conditions further complicate and add cost to care.
Medicare covers 56% of the health spending for duals, Medicaid picks up the tab for gaps in Medicare’s coverage (such as long-term care or prescription drug coverage). Breaking down the 300 billion dollar cost of duals, we find:
- According to CBO, Duals represent 13% of the total Medicare and Medicaid population, but account for 34% of the total cost of these programs.
- For Medicare, 18% of the entire population is dual eligible (8.28 million individuals) and accounts for nearly 27% of total Medicare program spending.
- CBO has also stated that for Medicaid, 15% of the population is dual eligible and accounts for 39% of the costs in that program.
- Duals are responsible for 27% of total long-term care expenditures.
- Annual spending for a single dual eligible consumer averages over $19,400 and can exceed $38,500 if more than one mental condition is present (20% of duals meet these criteria). PMPMs (per member per month) for a dually eligible member can easily exceed $3,500, which is often more than three times the cost of a healthy senior individual. A large number of duals suffer from severe physical and mental challenges requiring extensive support services. As shown below, mental illnesses including schizophrenia, Alzheimer’s and other forms of dementia, stroke, congestive heart failure, and cerebral palsy are more prevalent with duals than in the non-dual eligible Medicare populations.
- Patients who need long term institutional care consume over $56,000 a year in healthcare resources and with 20% of duals living in an institutionalized setting (and 16% living in nursing homes), they are among the most expensive to care for on a per capita basis.
- Three million children are part of the dual eligible population, and many of them have special care needs, which require close monitoring in order to avoid unnecessary hospitalization.
In the coming years, the dual eligible population, along with their associated costs, is poised to grow. Under the Patient Protection and Affordable Care Act, Medicaid expansion will increase enrollment by 40% up to 24 million adults. Without initiatives to address the complex and costly care coordination needs of the Medicaid population, costs and spending will grow. Given the size of the duals population and their complex care needs, along with the lack of care coordination between the federally-run Medicare and state-run Medicaid programs, governments and private insurers are increasingly shifting attention to initiatives that improve care, lower costs, and reduce waste and patient abuse. This shift is resulting in opportunities for innovative businesses to win large care management contracts.
Let us know what you think.